Urinary tract infections (UTIs) are among the most common bacterial infections affecting individuals of all ages. While many people experience a single UTI in their lifetime, others face recurrent UTIs, defined as having two or more infections within six months or three or more in a year. Understanding the causes and methods for recurrent UTI prevention can significantly improve the quality of life and reduce the need for frequent medical interventions.
What Causes Recurrent UTIs?
Recurrent UTIs often occur due to a combination of factors. Identifying these factors is critical to developing an effective prevention strategy.
- Bacterial Persistence
- Some strains of Escherichia coli(E. coli), the bacteria responsible for most UTIs, can attach to the walls of the urinary tract, forming biofilms that resist antibiotic treatment.
- These bacteria can remain dormant and later cause reinfection.
- Anatomical Factors
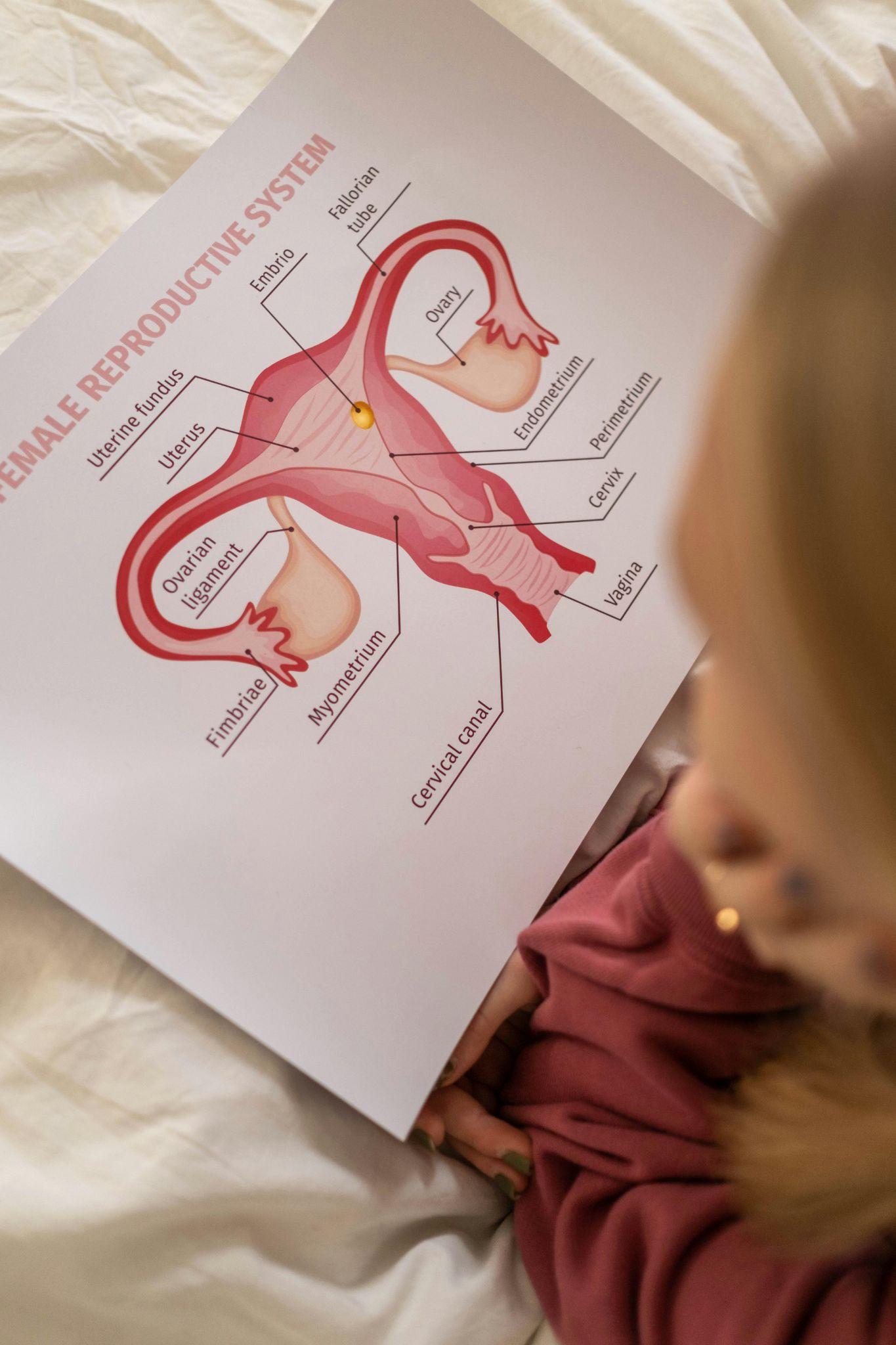
- Women are more susceptible due to a shorter urethra, which allows bacteria to reach the bladder more easily.
- Conditions such as kidney stones, bladder prolapse, or structural abnormalities of the urinary tract can increase the risk.
- Hormonal Changes
- Postmenopausalwomen often experience decreased estrogen levels, leading to changes in the vaginal microbiome and increased susceptibility.
- Sexual Activity
- Sexual intercourse can introduce bacteria into the urinary tract, particularly in individuals prone to recurrent UTIs.
- Other Contributing Factors
- Poor hygiene practices.
- Use of spermicides or diaphragms, which may disrupt the natural balance of bacteria.
- Chronic medical conditions such as diabetes that impair immune response.
- Incomplete emptying of the bladder, often associated with neurogenic bladder or certain medications.
Preventing Recurrent UTIs

Recurrent UTI prevention requires a multifaceted approach that combines lifestyle changes, medical interventions, and ongoing monitoring. Here are some evidence-based strategies to reduce the likelihood of recurrence.
Lifestyle Modifications
1. Stay Hydrated
- Drinking plenty of water helps flush bacteria from the urinary tract, reducing the risk of infection.
- Aim for at least 6-8 glasses of water daily.
2. Practice Proper Hygiene
- Wipe from front to back after using the restroom to avoid transferring bacteria to the urethra.
- Avoid using harsh soaps or douches that may disrupt the natural microbiome.
3. Urinate Frequently
- Avoid holding urine for long periods, as this can allow bacteria to multiply in the bladder.
- Empty the bladder fully each time.
4. Post-Sexual Activity Habits
- Urinate shortly after intercourse to flush out bacteria introduced during sexual activity.
- Consider avoiding spermicides if prone to UTIs.
5. Dietary Adjustments
- Include foods that promote urinary health, such as cranberry juice or supplements, which may prevent bacteria from adhering to the urinary tract lining.
- Probiotic-rich foods, such as yogurt, may help maintain a healthy balance of bacteria.
6. Wear Breathable Clothing
- Opt for loose-fitting, cotton underwear to reduce moisture and heat around the genital area, which can promote bacterial growth.
- Avoid tight pants or synthetic fabrics that may trap moisture.
Medical Interventions

1. Prophylactic Antibiotics
- In some cases, doctors may recommend low-dose antibiotics taken daily or after specific triggers, such as sexual activity.
- This approach can reduce the frequency of infections but should be closely monitored to prevent antibiotic resistance.
2. Vaginal Estrogen Therapy
- Postmenopausal women may benefit from topical estrogen, which helps restore the vaginal microbiome and reduce the risk of recurrent infections.
- Research has shown that estrogen therapy can improve the thickness and elasticity of the vaginal lining, creating a less hospitable environment for bacteria.
3. Vaccination
- Emerging vaccines targeting UTI-causing bacteria are being studied and may offer long-term prevention.
- These vaccines aim to train the immune system to recognize and combat specific bacterial strains, reducing recurrence rates.
4. Non-Antibiotic Therapies
- D-mannose, a sugar found in cranberries, may prevent E. coli from adhering to the urinary tract.
- Studies suggest that D-mannosecan be as effective as some antibiotics for preventing recurrent UTIs in certain populations.
- Methenamine, an antiseptic, can prevent bacterial growth in the bladder.
- Methenamine is particularly useful for patients who cannot tolerate antibiotics or wish to avoid long-term antibiotic use.
5. Addressing Underlying Conditions
- Treating conditions such as kidney stones, diabetes, or bladder dysfunction can reduce UTI recurrence.
- For example, managing blood sugar levels in diabetics has been shown to lower UTI risk by improving overall immune function.
6. Intravesical Therapy
- Intravesical therapy involves directly delivering treatment into the bladder through a catheter. This approach may help those with persistent or severe infections.
- It can include antibiotics, anti-inflammatory agents, or other medications tailored to the individual’s needs.
Advanced Prevention Methods
1. Personalized Medicine
- Genetic testing can identify specific bacterial strains and guide targeted treatment strategies.
- Microbiome analysis helps determine imbalances that contribute to recurrent UTIs.
2. Innovative Medical Devices
- Catheter modifications with antibacterial coatings can help individuals who require catheterization.
- Bladder instillations deliver medications directly to the bladder to prevent bacterial colonization.
3. Behavioral Therapy
- Pelvic floor physical therapy may benefit individuals with incomplete bladder emptying.
- Behavioral training can improve urinary habits and reduce UTI risk.
Complications of Recurrent UTIs
Without proper management, recurrent UTIs can lead to serious health problems, including:
- Kidney Infections:Repeated infections can spread to the kidneys, causing pyelonephritis, which may lead to long-term damage.
- Antibiotic Resistance:Overuse of antibiotics can result in drug-resistant bacterial strains, complicating future treatment.
- Quality of Life Impacts:Persistent discomfort, frequent doctor visits, and disruption of daily activities can affect emotional and physical well-being.
When to See a Doctor
While some UTIs can be managed with home remedies or over-the-counter treatments, recurrent UTIs require medical attention. It is important to consult a healthcare provider if:
- Symptoms persist despite treatment.
- There are signs of kidney infection, such as back pain, fever, or chills.
- UTIs occur frequently within a short time frame.
- You experience unusual symptoms, such as blood in the urine or severe pelvic pain.
A healthcare provider can perform diagnostic tests, such as urinalysis or urine cultures, to identify the underlying cause and recommend a personalized treatment plan.
Tips for Long-Term Management
Preventing recurrent UTIs often requires sustained efforts and ongoing communication with healthcare providers. Here are additional tips:
- Maintain Regular Checkups:Scheduling periodic visits with a healthcare provider ensures that any potential complications or patterns are detected early. Regular follow-ups also provide an opportunity to discuss the effectiveness of current prevention strategies and adjust them as needed.
- Track Symptoms:Keeping a detailed record of symptoms, frequency, and potential triggers can be invaluable. This information helps in identifying patterns and tailoring preventive measures to individual needs.
- Limit Antibiotic Use:Overuse of antibiotics can contribute to resistance and other side effects. Patients should explore alternatives and use antibiotics only when absolutely necessary, under a doctor’s guidance.
- Support Immune Health:Adopting a healthy lifestyle that includes regular exercise, a balanced diet rich in vitamins and antioxidants, and adequate sleep can enhance the body’s natural defense mechanisms. Managing chronic conditions, such as diabetes, is also crucial in reducing the risk of infections.
- Consider Preventive Therapies:Discuss with a healthcare provider whether long-term solutions like D-mannose supplements, vaginal estrogen, or Methenamine therapy are appropriate.
- Stay Educated:Staying informed about the latest advancements in UTI prevention can empower individuals to make proactive decisions. Patients may benefit from joining support groups or forums to share experiences and tips.
- Collaborate with Specialists: If UTIs persist despite preventive measures, consulting a specialist, such as a urologist or gynecologist, may uncover less common contributing factors, such as structural abnormalities or rare infections.
My Dr’s Note: Simplifying Medical Documentation
Recurrent UTIs are a common and often frustrating issue that can significantly impact daily life. Understanding the causes and implementing evidence-based strategies for recurrent UTI prevention is key to reducing their frequency and severity.
Early intervention and personalized treatment can help minimize complications and improve outcomes. For individuals needing assistance with medical documentation, such as online doctor’s notes for work or school, or FMLA certification services, My Dr’s Note is here to provide medical documentation for leave to help those managing ongoing health concerns.
Contact us today at My Dr’s Note for more information!


